I’ve been asked about Vicodin and Percocet more times than I can count, and honestly, it makes sense.
Both are powerful prescription opioids that doctors reach for when pain becomes unbearable, whether it’s post-surgery discomfort or chronic conditions. But here’s the thing: even though they’re in the same medication family, they’re not identical twins.
Different active ingredients mean different effects, risks, and considerations for your body. If you’ve ever wondered which one might be prescribed for you, or why your doctor chose one over the other, I’m here to walk you through it.
We’ll see how they work, what sets them apart, potential side effects, and how to use them safely. Remember, this is for educational purposes only; always consult your healthcare provider for personalized medical advice.
What is Vicodin?
Vicodin is a combination medication that pairs hydrocodone, an opioid pain reliever, with acetaminophen, the active ingredient in Tylenol.
Doctors typically prescribe it for moderate to moderately severe pain; think dental procedures, injuries, or post-operative recovery.
The hydrocodone component works by binding to opioid receptors in your brain and spinal cord, essentially changing how your body perceives and responds to pain. Meanwhile, the acetaminophen enhances this effect and helps reduce fever.
Vicodin comes in various tablet strengths, allowing healthcare providers to tailor the dosage to your specific pain level and medical needs. It’s a controlled substance due to its potential for dependence.
What is Percocet?
Percocet combines oxycodone, a potent opioid analgesic, with acetaminophen to tackle moderate to severe pain. It’s commonly prescribed after surgeries, significant injuries, or trauma when pain management becomes critical.
Oxycodone works similarly to hydrocodone by attaching to opioid receptors in your central nervous system, but it’s often considered stronger milligram-for-milligram in certain situations.
The added acetaminophen boosts the pain-relieving effects while also addressing inflammation and fever. Percocet is available in multiple tablet formulations with varying oxycodone and acetaminophen ratios, giving doctors flexibility in prescribing the appropriate strength.
Like Vicodin, it’s a Schedule II controlled substance, reflecting its high potential for abuse and addiction.
Key Differences Between Vicodin and Percocet
When choosing between these two medications, understanding their differences becomes crucial.
While they share similarities as opioid-acetaminophen combinations, the distinctions in their active ingredients, potency, and how your body processes them can significantly impact your pain management experience.
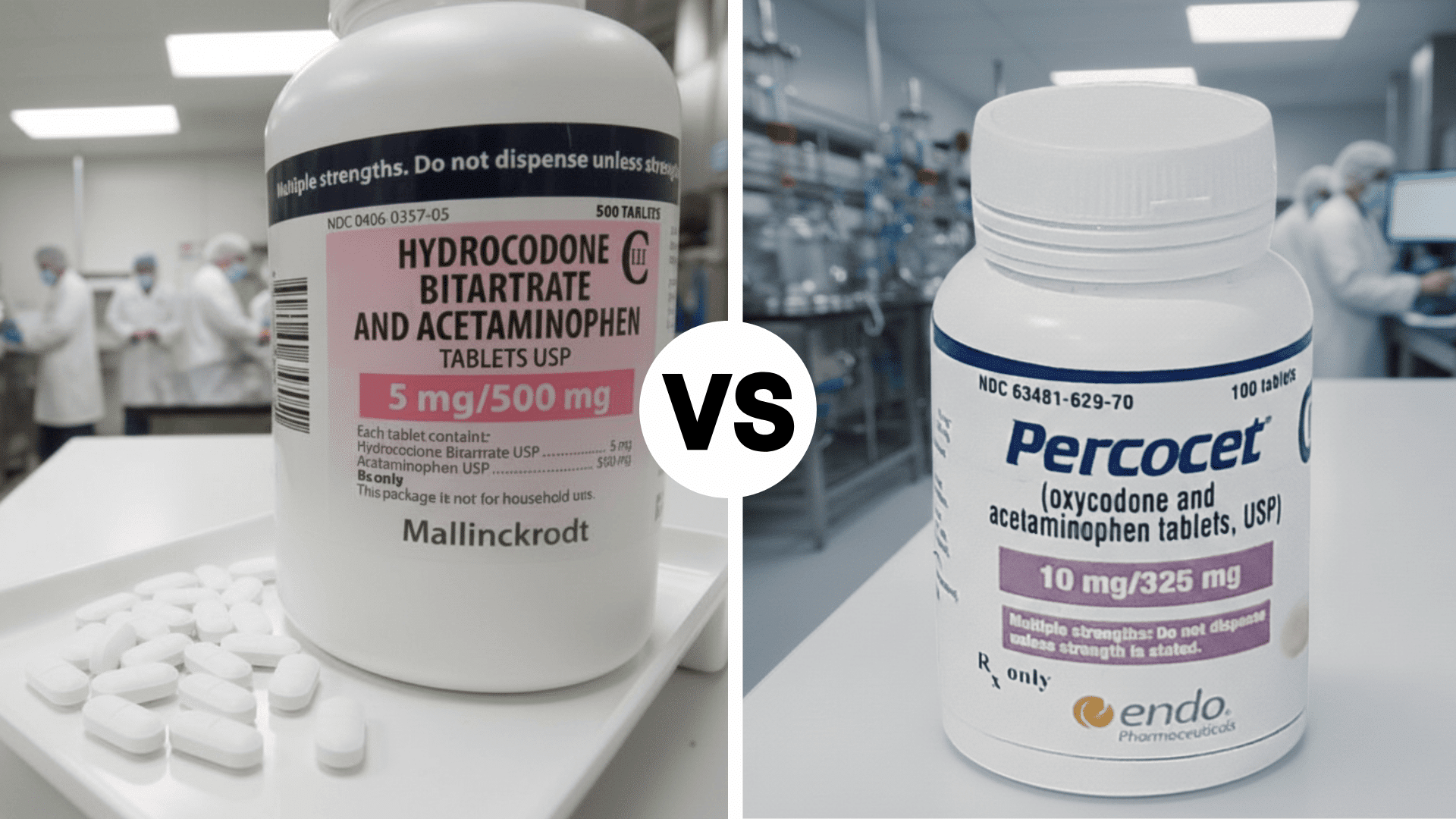
1. Active Ingredients (Hydrocodone vs. Oxycodone)
The fundamental difference lies in their opioid components. Vicodin contains hydrocodone, a semi-synthetic opioid derived from codeine, while Percocet uses oxycodone, which comes from thebaine.
Though both bind to the same opioid receptors, their chemical structures differ slightly, leading to variations in how they interact with your body.
This molecular distinction influences everything from potency to side effect profiles, making each suitable for different pain scenarios.
2. Strength and Effectiveness
Oxycodone in Percocet is generally considered more potent than hydrocodone in Vicodin when comparing equivalent doses.
Research suggests oxycodone has greater strength, though individual responses vary significantly. This doesn’t automatically make Percocet “better”: it simply means doctors might prescribe lower doses of oxycodone to achieve similar pain relief.
Your personal pain severity, tolerance, and medical history ultimately determine which medication works more effectively for you.
3. Onset & Duration of Action
Both medications typically begin working within less than an hour after taking them. Their effects last for several hours, providing similar relief windows.
The difference comes down to metabolism; your liver processes these drugs through different enzymatic pathways, which can affect how quickly they work and how long they last in your system, depending on your unique genetic makeup.
4. FDA Scheduling and Control
Both Vicodin and Percocet are classified as Schedule II controlled substances by the DEA, placing them in the highest category for medications with accepted medical use.
This classification reflects their significant potential for abuse, dependence, and addiction. Prescriptions require special handling; no refills are allowed, and doctors must provide new prescriptions for each fill.
This strict regulation aims to prevent misuse while ensuring patients with legitimate pain needs have access.
5. Cost and Availability
Generic versions of both medications are widely available and significantly cheaper than brand names. Prices vary depending on your insurance, pharmacy, and dosage strength, but generics typically range similarly in cost.
Insurance coverage usually treats them comparably since both are Schedule II opioids. However, individual pharmacies may have different stock levels based on local prescribing patterns.
Your doctor’s prescription and your pharmacy’s inventory often matter more than inherent availability differences between the two.
Similarities Between Vicodin and Percocet
Despite their differences, Vicodin and Percocet share remarkable similarities.
Both combine an opioid pain reliever with acetaminophen, creating a dual-action approach to pain management. They carry identical risks: dependence, addiction, respiratory depression, and potential overdose are concerns with both medications.
The acetaminophen component also poses liver damage risks if you exceed recommended doses or combine them with alcohol.
Doctors prescribe them for overlapping conditions involving moderate to severe pain, and both require careful monitoring and adherence to prescribed dosages.
They’re subject to the same strict regulations, and both can cause similar side effects like drowsiness, constipation, and nausea. Essentially, they’re more alike than different.
Side Effects of Vicodin vs Percocet
Both medications come with a range of side effects due to their opioid and acetaminophen components.
While many effects overlap, some patients experience variations in intensity or frequency depending on which medication they’re taking.
| Side Effect Category | Vicodin (Hydrocodone) | Percocet (Oxycodone) |
|---|---|---|
| Common Side Effects | Drowsiness, dizziness, nausea, constipation, lightheadedness | Drowsiness, dizziness, nausea, constipation, lightheadedness |
| Sedation Intensity | Moderate sedation reported by most users | Some patients report stronger sedation and drowsiness |
| Gastrointestinal Issues | Constipation, stomach discomfort, vomiting | Constipation, stomach discomfort, vomiting (may be more pronounced) |
| Cognitive Effects | Confusion, impaired thinking, mood changes | Confusion, impaired thinking, mood changes (potentially more intense) |
| Respiratory Impact | Slowed breathing, especially at higher doses | Slowed breathing, especially at higher doses |
| Liver Toxicity Risk | High risk if acetaminophen limits exceeded or combined with alcohol | High risk if acetaminophen limits exceeded or combined with alcohol |
| Allergic Reactions | Rash, itching, swelling (rare but possible) | Rash, itching, swelling (rare but possible) |
Never exceed prescribed doses of either medication, as the acetaminophen component can cause severe, potentially fatal liver damage when misused or combined with alcohol. If you experience difficulty breathing, extreme drowsiness, or signs of an allergic reaction, seek emergency medical attention immediately.
Risks & Warnings

Understanding the serious risks associated with Vicodin and Percocet is essential for safe use.
Both medications carry significant warnings that shouldn’t be taken lightly, from addiction potential to life-threatening overdose scenarios.
1. Dependence & Addiction
Both medications have high abuse potential as Schedule II controlled substances.
Physical dependence can develop even with prescribed use, causing withdrawal symptoms if stopped abruptly. Psychological addiction, characterized by cravings and compulsive use, poses serious risks.
Your body adapts to these drugs over time, potentially requiring higher doses for the same effect. Never increase dosages without medical supervision, and always discuss tapering plans with your doctor when discontinuing.
2. Overdose Risks
An overdose is life-threatening with both medications. The opioid component causes severe respiratory depression, potentially stopping your breathing.
This risk multiplies when combined with alcohol, benzodiazepines, or other depressants. Warning signs include extreme drowsiness, pinpoint pupils, cold skin, and shallow breathing.
If overdose is suspected, call emergency services immediately; naloxone can reverse opioid overdoses if administered quickly.
3. Acetaminophen Overuse
Exceeding daily acetaminophen limits can cause acute liver failure, which can be fatal or require transplantation.
Risk increases with alcohol use, other acetaminophen-containing products, or existing liver problems. Many over-the-counter medications contain acetaminophen; always check labels.
Never double-dose, thinking more provides faster relief. Your liver processes limited amounts safely; exceeding that threshold causes irreversible damage.
4. Who Should Avoid Use?
Certain individuals face heightened risks with these medications and should avoid them or use them only under careful medical supervision:
- People with Liver Disease: Acetaminophen can worsen liver damage in those with compromised liver function.
- Respiratory Condition Patients: Asthma, COPD, or sleep apnea increases the risk of dangerous breathing complications.
- Substance Use History: Past or current addiction significantly raises abuse and dependence potential.
- Pregnant or Breastfeeding Women: Both drugs can harm developing babies and cause newborn withdrawal.
- Kidney Disease Patients: Impaired kidney function affects medication processing and elimination.
- Those on Interacting Medications: MAO inhibitors, sedatives, or muscle relaxants create dangerous combinations.
Always provide a complete medical history to your healthcare provider before starting either medication. Honest communication ensures safer prescribing and better pain management.
Which is Stronger: Vicodin or Percocet?
When it comes to raw potency, Percocet is generally considered stronger than Vicodin due to oxycodone’s greater effectiveness compared to hydrocodone.
However, “stronger” doesn’t automatically translate to “better” for your situation. The right medication depends entirely on your specific pain level, medical history, how your body metabolizes drugs, and your doctor’s clinical judgment.
Some patients respond better to hydrocodone despite its lower potency, while others need oxycodone’s increased strength.
Your healthcare provider weighs multiple factors, including side effect tolerance and addiction risk, when deciding which medication suits you best. Strength is just one piece of the puzzle.
Safer Use & Alternatives
If you’re prescribed Vicodin or Percocet, using them responsibly is critical to minimizing risks.
Additionally, exploring non-opioid alternatives can help you manage pain effectively while avoiding the dangers associated with long-term opioid use.
- Follow Prescribed Dosages Exactly: Never take more than directed, don’t crush or chew tablets, and avoid mixing with alcohol or other sedatives.
- Consider Non-Opioid Pain Relievers First: NSAIDs like ibuprofen or naproxen can effectively manage moderate pain without addiction risks.
- Explore Physical Approaches: Physical therapy, acupuncture, massage, and targeted exercises address pain at its source rather than just masking symptoms.
- Use Opioids for Short-Term Relief Only: Reserve these medications for acute pain situations rather than chronic conditions that require ongoing management.
- Discuss Comprehensive Pain Management Plans: Work with your doctor on multimodal strategies combining medication, lifestyle changes, and therapeutic interventions for sustainable relief.
The safest approach combines responsible medication use with alternative pain management strategies tailored to your unique needs and circumstances.
Resources & References
For more detailed information and support, I recommend exploring these trusted resources.
The FDA medication guides provide comprehensive details about prescription opioids. The CDC’s opioid prescribing guidelines offer evidence-based recommendations for safe use.
MedlinePlus from the National Institutes of Health has extensive fact sheets on both hydrocodone and oxycodone.
If you or someone you know is struggling with opioid misuse, SAMHSA’s National Helpline at 1-800-662-4357 provides free, confidential support available around the clock.
The Bottom Line
Managing pain safely requires understanding what you’re putting into your body. While both Vicodin and Percocet can provide crucial relief when used responsibly, they’re not without serious risks.
I’ve walked you through their differences, similarities, and safety considerations so you can have informed conversations with your healthcare provider.
Remember, these medications are powerful tools meant for specific situations, not everyday solutions. Your pain management experience is personal, and finding the right approach takes patience and professional guidance.
Have questions or experiences you’d like to share about pain management? Drop a comment below; I’d love to hear your perspective and continue this important conversation together.