If you’re here because someone you know has taken too many benzos, or you’re worried about yourself, I want you to know this is a serious situation that needs immediate attention.
I’ve put together this guide to help you recognize the warning signs of a benzodiazepine overdose and understand what steps to take next.
We’ll walk through the symptoms you should watch for, the risk factors that increase danger, how overdoses are treated in medical settings, and most importantly, when it’s time to call for emergency help.
While I’m here to provide you with clear, actionable information, please remember this article is for educational purposes only and should never replace professional medical care.
What is a Benzodiazepine / “Benzo” Overdose?
Benzodiazepines are prescription medications that slow down your central nervous system. You might know them by names like Valium (diazepam), Xanax (alprazolam), Klonopin (clonazepam), or Ativan (lorazepam).
Doctors typically prescribe them for anxiety, panic disorders, seizures, or insomnia because they have a calming effect on your brain and body.
An overdose happens when you take more than your body can safely process.
This can occur by taking too much of the medication at once, or, and this is critically important, by combining benzos with other substances that depress your central nervous system, like alcohol, opioids, or certain sleep medications.
Understanding the Real Risk of Benzo Overdoses
Let me be straight with you about the actual danger level here, because the statistics tell a crucial story.
- Deaths from Single-Drug Benzo Overdoses Occur Infrequently: Your body can typically handle high doses if no other substances are involved.
- Nearly 70% of Benzo Deaths in 2023 Also Involved Illicitly Manufactured Fentanyl: Mixing turns the situation into a life-threatening emergency.
- 84% of Benzo-Involved Overdose Deaths from 2000-2019 Also Involved Opioids: The vast majority of fatalities happen when substances are combined.
- Co-Use With Opioids Increases Death Risk 10-Fold: One study found patients on both medications had ten times higher overdose death rates.
- Only 9% of Benzo Deaths Didn’t Involve Other Substances: Pure benzodiazepine deaths without opioids, alcohol, or other drugs are the exception.
- 10,870 Benzo-Involved Deaths Occurred in 2023: This represents a significant public health concern requiring immediate response.
What you need to understand is this: if someone has taken benzos alone, the situation is concerning but often manageable with medical care.
However, if there’s any possibility they’ve mixed benzos with opioids, alcohol, or other depressants, you’re looking at a genuine medical emergency where every second counts.
Early & Mild Symptoms of Benzo Overdose

Recognizing the early warning signs of a benzodiazepine overdose can make all the difference in getting help before the situation becomes critical.
Here’s what I need you to watch for in someone who may have taken too much.
1. Excessive Drowsiness, Sedation, or “Sluggish” Behavior
This goes beyond normal tiredness. The person might struggle to stay awake even in situations where they’d normally be alert, move in slow motion, or respond to questions with significant delays.
Their eyes may appear heavy-lidded, and they might nod off repeatedly during conversation. You’ll notice they seem unusually lethargic and lack their typical energy or responsiveness, appearing almost disconnected from their surroundings.
Why You Mustn’t Ignore This Sign: Extreme sedation can quickly progress to unconsciousness and respiratory depression, especially if other substances are involved.
2. Confusion or Disorientation
The person may seem lost or unable to understand where they are, what time it is, or who’s around them. They might ask the same questions repeatedly, give answers that don’t make sense, or struggle to follow simple conversations.
You may notice them appearing bewildered, having difficulty recognizing familiar people or places, or showing poor judgment in situations where they’d normally think clearly.
Why You Mustn’t Ignore This Sign: Cognitive impairment indicates the drug is significantly affecting brain function and can worsen rapidly.
3. Slurred Speech, Impaired Coordination & Balance
Their words may sound mushy or unclear, as if they’re struggling to form sentences properly. Walking becomes unsteady; they might stumble, sway, or need to hold onto furniture or walls for support.
Fine motor skills deteriorate, making simple tasks like picking up objects or buttoning clothing difficult. This loss of coordination, called ataxia, makes them appear intoxicated even without alcohol involvement.
Why You Mustn’t Ignore This Sign: Severe coordination problems increase fall risk and indicate advancing central nervous system depression.
4. Rapid Eye Movements or Blurred Vision
You might notice their eyes moving back and forth involuntarily in a jerky pattern, known as nystagmus. They may complain that their vision is blurry, doubled, or that they can’t focus on objects properly.
Some people describe feeling like the room is spinning or that they can’t track movement with their eyes. This symptom varies depending on which benzodiazepine was taken.
Why You Mustn’t Ignore This Sign: Visual disturbances signal significant neurological effects and can lead to dangerous accidents or injuries.
Severe / Life-Threatening Symptoms

When benzodiazepine overdose progresses to these severe symptoms, you’re in emergency territory where minutes matter.
If you observe any of the following signs, call emergency services immediately; don’t wait to see if things improve.
5. Deep Sedation, Stupor, or Coma
The person becomes profoundly unresponsive, going beyond drowsiness into a state where they barely react to stimuli or don’t respond at all.
In stupor, they might only respond to painful stimuli like a firm pinch. In a coma, even painful stimulation produces no meaningful response.
Their body appear limp, and attempts to communicate with them fail completely. This represents severe central nervous system depression where the brain’s normal functions are critically compromised.
What This Means for Survival: This level of unresponsiveness indicates life-threatening brain depression requiring immediate emergency medical intervention.
6. Respiratory Depression
Breathing becomes dangerously slow, shallow, or irregular; you might count fewer than twelve breaths per minute or notice long pauses between breaths.
Their chest movements may be barely visible, and the breaths they do take seem weak or ineffective.
Skin color may start changing to pale, bluish, or grayish tones, especially around the lips and fingernails, indicating insufficient oxygen. This is the most dangerous complication of benzodiazepine overdose.
What This Means for Survival: Respiratory failure is the primary cause of death in benzodiazepine overdoses and requires immediate emergency response.
7. Cardiovascular Effects
Heart rate drops significantly below normal, blood pressure falls dangerously low, and in severe cases, the heart’s electrical system can malfunction, causing abnormal rhythms.
You might notice a weak pulse that’s difficult to find, cold and clammy skin, or the person appearing shocked. Their extremities may feel cool to the touch.
While less common than respiratory issues in pure benzo overdoses, cardiovascular complications become more likely when other substances are involved.
What This Means for Survival: Cardiac complications can lead to organ damage, shock, and death if not treated immediately in a hospital setting.
8. Loss of Consciousness
The person cannot be awakened, no matter how hard you try: calling their name loudly, shaking them, or applying painful pressure produces no response.
Their eyes remain closed, they don’t make purposeful movements, and they show no awareness of their environment.
This is distinctly different from deep sleep because normal methods of waking someone completely fail. It represents a critical level of brain function impairment.
What This Means for Survival: Unconsciousness leaves the person vulnerable to choking, aspiration, and airway obstruction; call emergency services immediately.
9. Seizures
While uncommon in straightforward benzo overdoses, seizures can occur in certain situations, particularly if the person is physically dependent on benzodiazepines and suddenly stops taking them, or if flumazenil is administered improperly.
You’ll see uncontrolled jerking movements, muscle rigidity, loss of consciousness, and possibly loss of bladder control. The person may bite their tongue or injure themselves during the convulsion.
What This Means for Survival: Seizures indicate severe neurological distress and can cause brain damage or death without immediate medical treatment.
Risk Factors & Co-Ingestions That Make Overdose Worse
Certain factors can transform a manageable benzo situation into a life-threatening emergency. Understanding these risk multipliers helps you assess the severity of the situation you’re facing.
- Combining With Alcohol, Opioids, or Barbiturates: Mixing benzodiazepines with other central nervous system depressants dramatically increases the risk of fatal respiratory depression.
- Advanced Age or Existing Breathing Problems: Older adults and people with lung conditions like COPD or sleep apnea are far more vulnerable to respiratory complications.
- Liver Impairment or Kidney Disease: Reduced organ function slows drug elimination, causing benzodiazepines to build up to dangerous levels in the body.
- High Doses or Long-Acting Benzodiazepines: Taking excessive amounts or using longer-lasting benzos like diazepam or clonazepam extends and intensifies the overdose effects.
- Rapid Dose Escalation or Pre-Existing Sedation: Quickly increasing doses or taking benzos while already drowsy from other medications compounds central nervous system depression.
The presence of even one risk factor can mean the difference between a close call and a tragedy.
What Happens Physiologically in an Overdose?
Understanding what’s happening inside the body during a benzodiazepine overdose can help you grasp why these symptoms occur and why immediate medical care is so critical.
Here’s what’s going on at a biological level:
| Physiological Effect | Body System | Mechanism | Result |
|---|---|---|---|
| Excess GABAergic Inhibition | Central Nervous System | Benzos amplify GABA, the brain’s calming neurotransmitter | Excessive brain activity suppression beyond therapeutic levels |
| Suppression of Respiratory Drive | Brainstem & Lungs | Breathing control centers become overly sedated | Dangerously slow or shallow respiration |
| Impaired Reflexes | Airway & Throat | Protective reflexes like coughing and swallowing weaken | Increased choking, aspiration, and airway obstruction risk |
| Cardiac & Vascular Effects | Heart & Blood Vessels | The heart’s electrical system and vessels are affected | Slowed heart rate, low blood pressure, abnormal rhythms |
These physiological changes explain why benzodiazepine overdoses become exponentially more dangerous when combined with other depressants; each substance compounds the suppression of vital life-sustaining functions.
How is a Benzodiazepine Overdose Diagnosed?
When you arrive at the emergency department, medical professionals follow a systematic approach to confirm benzodiazepine overdose and assess its severity.
Here’s what the diagnostic process typically involves:
- Clinical Assessment and Vital Signs: Doctors evaluate symptoms, consciousness level, respiratory rate, oxygen saturation, and blood pressure immediately upon arrival.
- Patient History Collection: Medical staff gather information about which benzodiazepine was taken, dosage amount, timing, and any co-ingested substances like alcohol or opioids.
- Toxicology Screening: Blood and urine tests detect benzodiazepines and other drugs in the system to confirm overdose and identify polysubstance use.
- Cardiac and Respiratory Monitoring: ECG tracks heart rhythm abnormalities while arterial blood gas analysis measures oxygen and carbon dioxide levels to assess lung function.
- Organ Function Testing: Liver and kidney function labs evaluate the body’s ability to metabolize and eliminate the drug from the system.
The diagnostic process happens quickly in emergency settings, with treatment often starting immediately based on clinical presentation rather than waiting for all test results to return.
Benzo Overdose: Treatment & Management
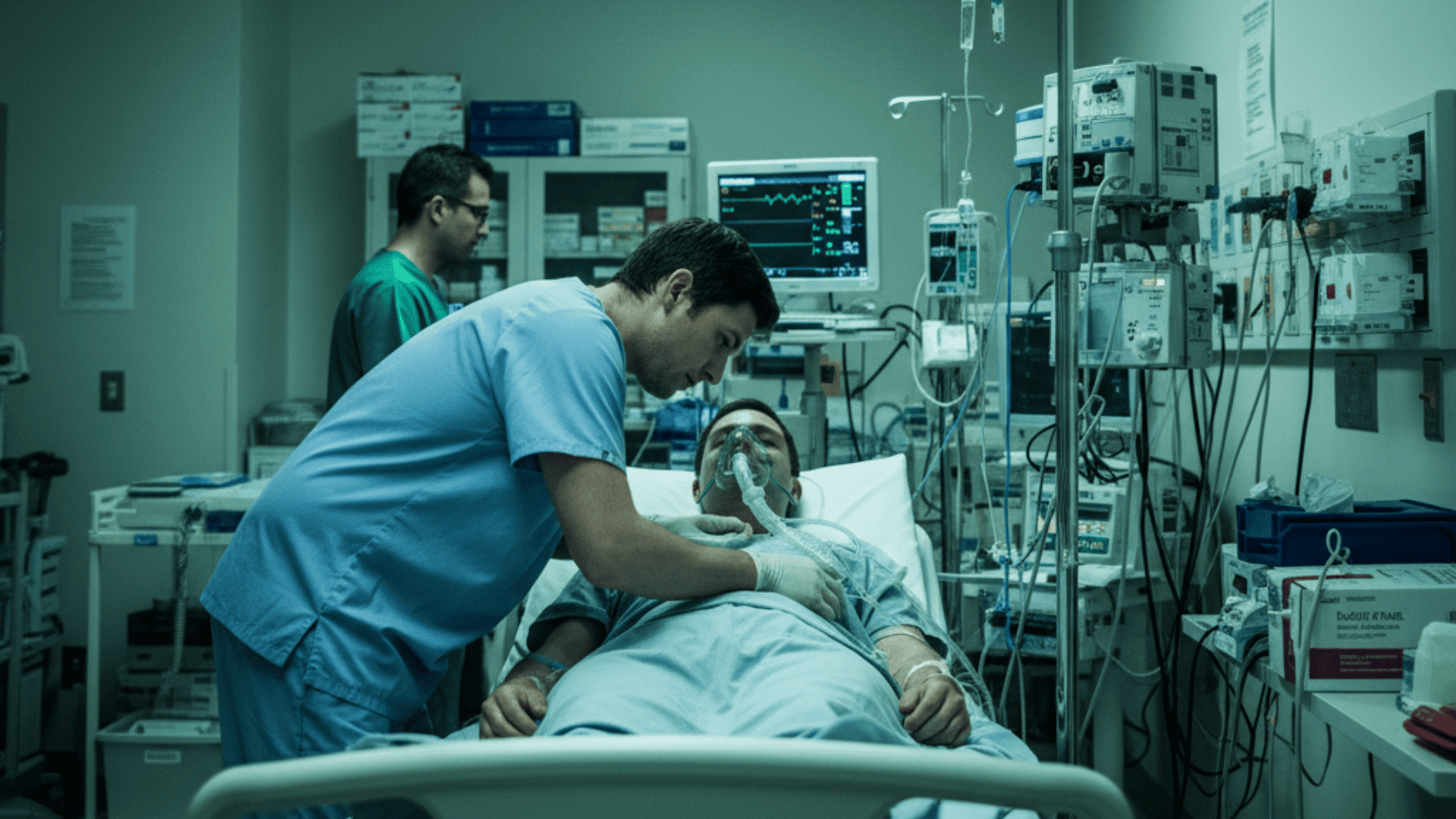
If someone you know is experiencing a benzodiazepine overdose, medical professionals have specific protocols to stabilize them and reverse the dangerous effects.
Here’s what happens once emergency care begins and the treatment options are available.
Supportive Care and Emergency Stabilization
The foundation of benzodiazepine overdose treatment focuses on keeping vital functions stable.
Medical teams immediately secure the airway, provide oxygen or ventilation support if breathing is compromised, and continuously monitor heart rate, blood pressure, and oxygen levels. Activated charcoal may be given if ingestion was recent to prevent further drug absorption.
IV fluids help maintain blood pressure, and medications called pressors are administered if hypotension becomes severe. Critical cases require intensive care unit monitoring.
Flumazenil Antidote: Use and Limitations
Flumazenil is a benzodiazepine antidote that can rapidly reverse overdose effects by blocking benzo receptors in the brain.
However, its use is controversial and limited due to serious risks; it can trigger dangerous seizures in people who regularly use benzodiazepines or who’ve taken seizure-lowering drugs. Doctors avoid flumazenil in mixed overdoses involving opioids, tricyclic antidepressants, or when a seizure history exists.
Most patients recover well with supportive care alone, making flumazenil necessary only in carefully selected cases where benefits outweigh risks.
Aftermath, Recovery, & Long-Term Considerations
Surviving a benzodiazepine overdose is just the beginning. There are important recovery aspects and potential complications that need attention in the hours, days, and weeks that follow.
- Residual Sedation and Cognitive Impairment: Drowsiness, confusion, and mental fog can persist for hours or days after overdose, especially with long-acting benzos.
- Withdrawal Risk in Chronic Users: abrupt cessation or flumazenil reversal in regular benzo users can trigger dangerous withdrawal symptoms, including seizures.
- Complications Monitoring: Ongoing assessment for aspiration pneumonia, brain damage from oxygen deprivation, and other respiratory depression consequences.
- Psychiatric Evaluation and Mental Health Support: Assessment determines if overdose was intentional and addresses underlying depression, anxiety, or suicidal ideation.
- Substance Use Treatment Programs: Connecting with addiction counseling, therapy, and support groups prevents future overdoses and addresses misuse patterns.
Recovery doesn’t end when you leave the hospital.
Following up with healthcare providers, attending therapy, and building a support network are key steps to prevent recurrence and address underlying issues that contributed to the overdose.
The Bottom Line
I’ve walked you through everything you need to recognize and respond to a benzodiazepine overdose, from the earliest warning signs to what happens in the emergency room.
The key takeaway? Never underestimate the danger of mixing benzos with other substances, and never hesitate to call for help when you suspect an overdose.
Knowledge saves lives, and now you have the information to act decisively in a crisis.
If you’ve experienced a benzo overdose or helped someone through one, I’d love to hear your story in the comments below. Your experience could help someone else recognize the signs when it matters most.






